Bone powder: The new generation of bone regeneration materials in implantology treatments
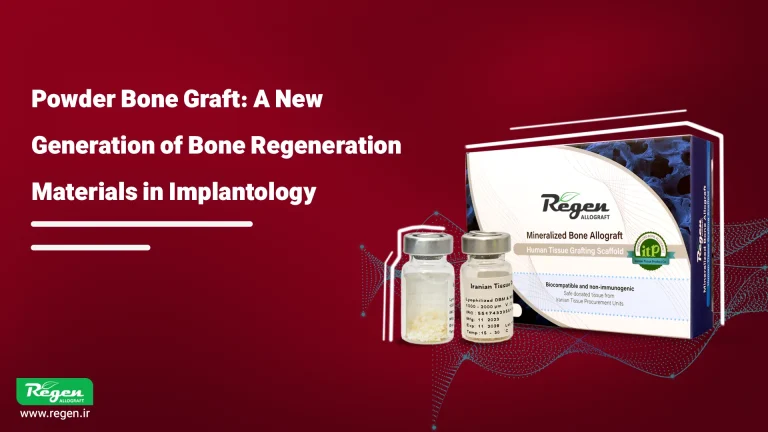
Table of contents
Introduction
The success of dental implant treatment depends not only on the quality of the implant and the surgeon’s skill but also on the quantity and quality of the host bone. In many patients—especially those who have been edentulous for a long time or suffer from bone resorption—the available bone volume is insufficient for implant placement. In such cases, the use of bone powder or other regenerative materials becomes essential to strengthen the bone foundation. Selecting the appropriate type of bone graft material plays a key role in the degree of bone regeneration, the long-term stability of the implant, and the overall treatment outcome.
Why Do We Need Bone Powder?
After tooth extraction, the alveolar bone gradually begins to resorb. This process may lead to a reduction in bone height or width, making implant placement impossible without prior regeneration. The main purpose of using bone powder is to provide a biological scaffold that supports the growth of osteogenic cells and promotes the formation of new bone tissue.
Bone graft materials not only maintain the required space but also gradually integrate and are replaced by the patient’s natural bone, contributing to implant stabilization.
Types of Bone Powder
Bone graft materials used in dentistry are generally classified into four main categories based on their origin:
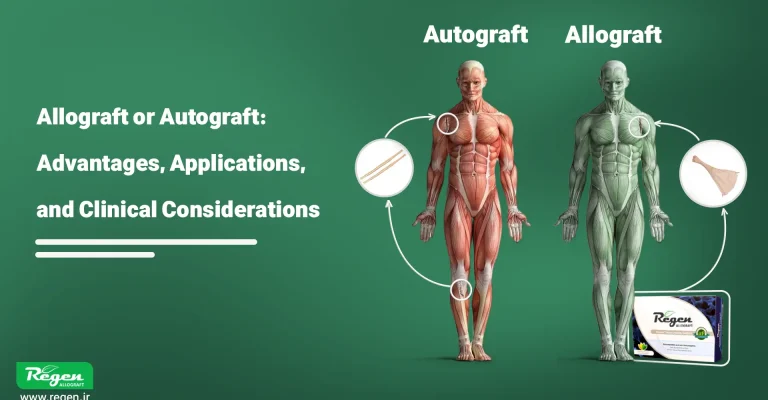
1. Autograft:
In the autograft method, bone is harvested from the patient’s own body—usually from the jaw or hip. It is the most biocompatible option; however, due to the need for a second surgical site, associated pain, cost, and limited available volume, its use is less common.
2. Allograft:
Allografts are obtained from donated human tissue, processed, and sterilized in a tissue bank. This type of bone powder (such as products from the Regen brand) is the most commonly used option in Iran. Allografts are highly biocompatible, eliminate the need for bone harvesting, and are available in different grades, making them widely used in implant surgeries.
3. Xenograft:
Xenografts are derived from animal sources (usually bovine). They possess a mineral composition similar to that of human bone and primarily exhibit osteoconductive properties. The most well-known example is Bio-Oss bone powder.
4. Synthetic or Alloplast:
These materials are made from mineral or ceramic compounds such as hydroxyapatite or β-TCP. They are biocompatible and safe but may have limited resorption rates or osteoinductive potential compared to natural grafts.

Key Features in Selecting Bone Powder
Choosing the right type of bone powder depends on multiple factors that directly affect the overall success of implant treatment:
1. Biocompatibility
The graft material must function without causing inflammatory responses or tissue rejection. Processed allografts such as Regen minimize immune reactions by removing cellular components and antigenic factors.
2. Osteoinduction
Some bone powders contain natural growth factors that stimulate stem cells to differentiate into osteoblasts. Demineralized bone matrices (DBM) demonstrate superior performance in this regard.
3. Osteoconduction
Bone powder should provide a three-dimensional scaffold with adequate porosity for cell growth and vascular infiltration. The greater the surface area, the faster the integration with the host bone.
4. Resorption Rate
A proper balance between resorption and new bone formation is crucial. Materials that resorb too quickly may disappear before new bone is formed, while slow-resorbing powders may delay the regeneration process.
5. Particle Size and Density
Coarser particles are more suitable for large-volume reconstructions, whereas finer particles are ideal for filling small defects. A combination of different particle sizes generally produces better results.
Effect of Bone Powder Type on Implant Success
The choice of bone powder directly influences several key factors in implant therapy:
1. Osseointegration
Successful mechanical stability of the implant depends on the integration between the implant surface and newly formed bone. Bone powders with high osteoinductive properties accelerate the osseointegration process.
2. Bone Volume Maintenance
In jawbone reconstruction, the type of graft material determines how much bone volume will be maintained over time. Slowly resorbing allografts are generally more effective in preserving bone volume.
3. Reduction of Post-Implant Bone Resorption
Studies have shown that using the appropriate bone powder significantly reduces peri-implant bone loss and improves the long-term survival of crowns and prosthetic restorations.
4. Aesthetic Outcome
In anterior jaw regions, complete and stable bone regeneration helps preserve the gingival contour and maintain harmonious aesthetic lines.
Common Examples in Bone Regeneration
A wide variety of bone powders are available in the Iranian market, each with specific properties.
For instance, domestically produced allograft powders such as Regen Bone Powder—with sterile processing and variable particle sizes—have proven to be reliable alternatives to imported products and are now widely used in jawbone and implant reconstruction procedures.
Key Features in Selecting Bone Powder
Selecting the appropriate type of bone powder depends on several factors that directly influence the overall success of the dental implant:
Biocompatibility
The bone powder must function without triggering inflammatory responses or tissue rejection. Processed allografts, such as Regen, minimize immune reactions to the lowest possible level.
Osteoinduction
Some bone powders contain natural growth factors that stimulate stem cells to differentiate into osteoblasts. Demineralized bone powders show superior performance in this regard
Osteoconduction
The bone powder should provide a three-dimensional scaffold with adequate porosity to support cell growth and vascular infiltration, facilitating faster integration with the host bone.
Resorption Rate
A balance between resorption and new bone formation is crucial. Powders that resorb too quickly or too slowly can negatively affect the bone regeneration process.
Particle Size and Density
Coarser particles are suitable for larger reconstructions, while finer particles are ideal for filling small defects. A combination of different particle sizes generally yields better results.
The Impact of Bone Powder Type on Implant Success
Osseointegration: Bone powders with high osteoinductive properties accelerate the integration of the implant with the surrounding bone.
Bone Volume Maintenance: Slowly resorbing bone powders are more effective in maintaining long-term bone volume.
Reduction of Post-Implant Bone Resorption: Using the appropriate bone powder helps minimize bone loss around the implant.
Aesthetic Outcome: Complete and stable bone regeneration preserves the gingival contour and ensures harmonious aesthetic lines.
Conclusion
The success of dental implant treatment is not limited to precise implant placement or the type of implant used; rather, the proper selection of bone powder as the regenerative foundation plays a vital role in the final outcome. Understanding the differences among various types of bone powders, being aware of their biological properties, and matching them to each patient’s specific condition can significantly enhance the likelihood of treatment success. Ultimately, close collaboration between the surgeon, prosthodontist, and the regenerative materials team is the key to achieving a stable, functional, and aesthetically pleasing implant.
Source:
Ferraz MP, et al. Bone Grafts in Dental Medicine: An Overview of Autografts, Allografts, and Xenografts. Materials. 2023;16(11):4117. DOI: 10.3390/ma16114117 (Authenticus.pt)
Gruskin E, et al. Demineralized Bone Matrix in Bone Repair: History and Use. Advanced Drug Delivery Reviews. 2012;64(12):1063–1077. DOI: 10.1016/j.addr.2012.06.008 (PubMed)
Zhao R, et al. Bone Grafts and Substitutes in Dentistry: A Review. Molecules. 2021;26(10):3007. DOI: 10.3390/molecules26103007 (PubMed)
Aludden HC, et al. Lateral Ridge Augmentation with Bio-Oss: A Systematic Review. International Journal of Oral and Maxillofacial Surgery. 2017;46(8):1030–1038. DOI: 10.1016/j.ijom.2017.03.008 (VBN)
Li Y, et al. Comparison of Osteogenic Effectiveness of Bio-Oss and Autogenous Grafts: A Meta-Analysis. British Journal of Oral and Maxillofacial Surgery. 2022;60(9):1094–1103. DOI: 10.1016/j.bjoms.2022.03.009 (PubMed)
How useful was this post?
Click on a star to rate it!
Average rating 0 / 5. Vote count: 0
No votes so far! Be the first to rate this post.
Relevant Posts

Free consultation
Do you need counseling?
The professional and specialized team at Allograft is ready to assist you