The Shell Technique with Allograft: From Cortical Plate to the Innovative Single-Screw Cortical Disk

Table of contents
Introduction: Defining a Strategy for Managing Uncontained Bone Defects
In the first part of this article series, we emphasized the critical importance of accurately diagnosing periodontal osseous defects (PODs) and their morphologic classification, particularly in extra-osseous lesions or non-containable defects lacking sufficient bony walls. These lesions, often presenting as severe horizontal alveolar ridge resorption, pose the greatest challenge in implantology reconstructions. The primary and decisive challenge in these cases is maintaining a stable space for osteogenic cell colonization and new bone matrix formation, while preventing mechanical collapse of the soft tissue over the graft.
Jawbone reconstruction is one of the most sensitive and challenging stages in implantology and periodontal treatments. As comprehensively discussed in the previous part of this article series, accurate diagnosis of periodontal osseous defects (PODs) and their classification into containable and non-containable defects form the cornerstone for selecting the appropriate technique. In cases of severe resorption and non-containable horizontal alveolar ridge defects, the primary challenge—often leading to volumetric failure—is the inability to maintain a stable space against pressure exerted by converging soft tissue.
The Shell Technique in implantology, using dental cortical allograft blocks or plates, has been introduced as a powerful biomechanical solution to overcome this challenge. The aim of this article is to provide a comparative review of the classic shell technique and to present and describe its innovative and simplified protocol—the modified shell technique with a single-screw cortical disc— a method that maximizes efficiency and simplicity in horizontal localized jawbone reconstruction.
Philosophy of the Shell Technique: Why Allograft and Rigid Barriers
In traditional guided bone regeneration (GBR) techniques using standard resorbable collagen membranes, the failure mechanism is straightforward. Thin membranes lacking the necessary mechanical strength cannot withstand the pressure exerted by a full-thickness flap and easily collapse. This collapse eliminates the space required for osteogenic cell colonization and angiogenesis, directly preventing the achievement of the desired bone width.
:Horizontal Bone Reconstruction Strategy
Allograft and Rigid Barrier
High Predictability with the Bone Frame Approach
Preferred Choice: Allograft
Allograft is considered the preferred graft material due to its biocompatibility, unlimited availability, and elimination of donor site morbidity.
Compensating Mechanical Deficiency with a Rigid Barrier
The use of cortical plates or cortical discs (Regen Allograft) compensates for the mechanical shortcomings of graft particulate by providing a rigid physical barrier.
Creating Exceptional Space Stability
This barrier, by creating a chamber or bone frame, provides exceptional space stability and protects the graft particles from external pressures.
Final Outcome: High Predictability✓
This approach ensures that the regenerated space is maintained throughout the healing period, providing high predictability in horizontal bone reconstruction.
Classic Shell Technique (with Cortical Plate): Biomechanical and Operational Challenges
In the classic shell technique, the surgeon uses a relatively large cortical plate. While this method remains the gold standard for extensive (segmental) reconstructions, it presents several challenges in localized reconstructions
Limitations of the Classic Shell Technique
1. Operational Complexity and Shapin:
The plate must be custom-cut and shaped to perfectly match the defect morphology. This intraoral trimming and adaptation process requires the use of diamond burs with ample irrigation, making it a time-consuming and delicate step that increases the risk of plate fracture.
2. Need for Multiple Fixations and Biomechanical Risk:
To ensure complete stability and prevent rotational or sliding micromovements of large plates, the use of at least two to four fixation screws is essential.
- Stress Concentration and Bone Resorption: Each screw creates a point of stress concentration in the host bone. A high number of screws can increase the risk of bone resorption around the screw heads, which may gradually compromise plate stability over time.
- Difficulty of Achieving Passive Fit: Placing multiple screws in the confined intraoral environment requires high precision to ensure the plate sits completely passively on the host bone. Any residual stress or gap at the plate–bone interface can lead to resorption or failed plate integration.
3. Increased Surgical Time and Trauma:
Intraoral fixation of large, multi-screw plates, especially in posterior regions or areas with pronounced jaw curvature, significantly increases surgical time, which is directly associated with a higher risk of contamination and postoperative swelling.
Innovation: Single-Screw Cortical Disc and Its Biomechanical Advantages
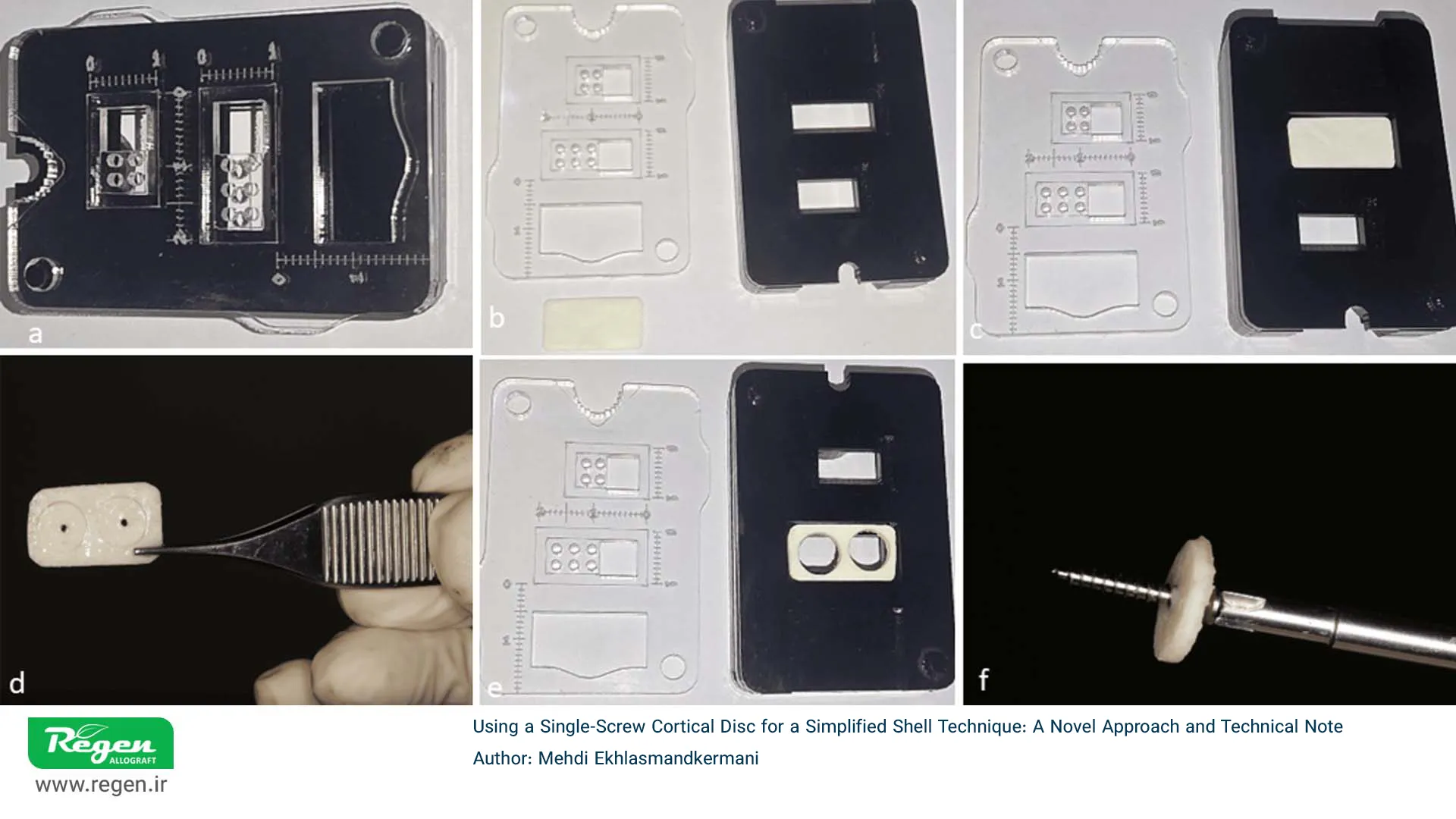
Steps for Fabrication and Preparation of the Single-Screw Cortical Disc Using a Dedicated Template — Adapted from the article Using a Single-Screw Cortical Disc for a Simplified Shell Technique by Dr. Mehdi Ekhlasmand-Kermani
This modified method replaces the rectangular plate with a circular cortical allograft disc (approximately 8 mm in diameter and 1.2–1.4 mm in thickness, similar to Regen Allograft discs) and achieves anti-rotational stability with a single screw by eliminating additional lever forces. This approach was introduced in 2025 as a simple and minimally invasive technique.
- Minimal Trauma and Ease of Execution: By eliminating the need for complex cutting and shaping, surgical time is significantly reduced, and the risk of damage to sensitive anatomical structures is lowered.
Preoperative Preparation (Extraoral Assembly): Precise Torque ControlOne of the key innovations is the extraoral preparation of the disc–screw assembly, which enhances precision and efficiency during surgery.
Precise Drilling and Heat Control
The central hole of the disc, 1.4 mm in diameter for a 1.6 mm screw, is created extraorally to prevent heat transfer and reduce the risk of osteonecrosis.
Screw and Driver (High-Torque Screw)
A self-tapping titanium screw with threads extending to the head provides sufficient torque for a secure disc–screw connection.
Precise extraoral preparation ensures torque accuracy and thermal control, leading to increased stability, reduced risk of fracture, and improved predictability of the restoration.
Hard tissue and graft material management: Precise surgical protocol and biological considerations
The success of this technique depends on strict adherence to the PASS principles (Preserve the Stable Space, Angiogenesis, Primary Space, Stable Clot).
Stimulating Biological Potential: The RAP Phenomenon and Angiogenesis
After the elevation of the full-thickness flap, the crucial step is the stimulation of bleeding and the biological potential of the host bone.
Regional Acceleratory Phenomenon (RAP): Creating multiple perforations or a corticotomy in the host cortical bone, by establishing communication with the bone marrow, activates the Regional Acceleratory Phenomenon (RAP). RAP is a physiological response that increases local blood flow, enhances the activity of osteoblast and osteoclast cells, and accelerates the rate of regeneration. These perforations provide the primary source of mesenchymal cells and new blood vessels for the graft.
Fixation Strength: Bi-Cortical Anchorage and Resistance to Micromovement
Bi-Cortical Fixation (engaging two cortical layers) is the biomechanical backbone of this technique. This fixation, by simultaneously engaging the screw in the buccal and lingual/palatal cortices, significantly increases the Primary Stability of the disc.
- Resistance to Micromovement: Bi-cortical stability enhances the resistance of the assembly against microscopic movements, which, according to the principles of Fracture Healing, are the primary enemy of bone repair. Minor movements in the graft area lead to the formation of fibrous tissue instead of bone.
- Screw Length Calculation: Calculating the precise screw length is vital for achieving accurate and safe bi-cortical fixation. The screw must cover not only the thickness of the disc and the graft space but also engage the opposing cortical bone by 1 to 2 mm to ensure three-dimensional stability, while simultaneously avoiding damage to posterior vital structures.
Bone Material Selection and Biological Enrichment Strategy
Graft selection in the sub-discal space must be based on the disc’s structural role (space maintenance) and the need for a slow-resorbing scaffold:
Cortical Allograft (Slow-Resorbing Scaffold):
Pure cortical allograft powder, due to its dense structure and slow resorption rate, provides a stronger and longer-lasting osteoconductive scaffold. This extended stability allows the cortical disc to maintain its structure throughout the healing period, preventing early graft resorption and volume loss. In most cases, FDBA with particle sizes of 500 to 1000 microns is used.

Use of Bone Graft Particulate in the Shell Technique with a Cortical Disk
Bone Conditioned Medium (BCM)
The combination of allograft particulate with locally derived growth factor–rich blood (BCM) provides an optimal biological environment. BCM is prepared from blood collected at the surgical site (via RAP) and autogenous chips (when available). This mixture enhances the graft potential from a purely osteoconductive material to a construct with osteogenic and osteoinductive properties, while also improving the stability of the initial blood clot.
Tension-Free Closure: The Key to Success
The most critical factor for success is proper soft tissue management and tension-free suturing to prevent early disk exposure. Disk exposure carries a high risk of infection and complete graft failure. This requires:
Periosteal Releasing Incision
- Performing a full-thickness releasing incision (Scorching) in the flap to allow coronal advancement and placement of the wound edges over the graft without any tension. This step requires soft tissue reconstruction extending at least 2 mm beyond the edge of the disk.
Membrane Coverage)
- The use of a resorbable collagen membrane over the disk–graft construct as a secondary protective layer and a cellular barrier is essential.
Suturing Technique:
- The use of double-layer suturing techniques (deep horizontal matrix and superficial interrupted sutures) to achieve a complete and stable seal.
Healing Phase, Integration Assessment, and Clinical Outcomes (Re-Entry)
This phase involves the completion of the healing process and the final assessment of treatment success and the integration of the allograft with the host bone.
Total Healing Duration:
- Typically, it takes 4.5 to 5 months for the transition from woven bone to lamellar bone to be completed, increasing the likelihood of disk integration with the host bone.
Disk Management in Re-Entry Surgery:
- The fixation screw is removed. Allograft disks have integrated with the new bone and do not need to be harvested (Cureus 2025 study).
Key Advantage:
- Disk integration provides a major advantage over the mandatory removal of titanium meshes.
Final Contouring:
- Any sharp edges, protrusions, or irregular margins should be carefully smoothed and contoured to prevent localized pressure and reduce the long-term risk of soft tissue dehiscence.
Clinical Comparison: Classic Shell Technique versus Single Disk
| Characteristics | Classic Shell with Plate | Shell Technique with Disc (Single Screw) |
|---|---|---|
| Number of Screws | 2 to 4 pieces (High Stress Concentration Risk) | 1 piece (Significant Reduction in Stress Concentration) |
| Surgery Duration | Longer (Complexity of Adaptation and Fixation) | Shorter (Extraoral Assembly) |
| Plate Fracture Risk | Higher (especially during bending and multiple fixations) | Significantly lower |
| Anatomical Adaptability | Limited (Requires extensive shaping) | High (Easy adaptation to local curvature) |
| Primary Reconstruction Goal | Extensive and Segmental Defects | Localized and Focal Defects |
| Need for Subsequent Removal | Yes (if complete integration is not achieved) | Usually not required (due to high integration rate) |
| Risk of Exposure | Moderate (due to flap stresses caused by the large plate) | Low (small volume and easy adaptation) |
Summary and Clinical Message
The modified shell technique with single-screw cortical disc represents a significant advancement in horizontal jawbone reconstruction. By eliminating multiple screws and simplifying fixation, it reduces surgical trauma while ensuring mechanical stability through bi-cortical fixation, ultimately enhancing clinical predictability.
Utilizing the Regen Allograft product portfolio—including cortical plates and cortical discs—surgeons can select complementary structures tailored to the extent and morphology of the defect, from segmental cases to localized lesions. This approach maintains spatial stability as a key success indicator.
According to Dr. Mehdi Akhlasmand’s recommendation, cortical discs represent an evolved version of cortical plates. While preserving their primary function of creating/maintaining space, they make the shell technique more efficient and less invasive.
References
How useful was this post?
Click on a star to rate it!
Average rating 5 / 5. Vote count: 1
No votes so far! Be the first to rate this post.
Relevant Posts

Free consultation
Do you need counseling?
The professional and specialized team at Allograft is ready to assist you