PASS Principles for Predicting Bone Regeneration Success in GBR
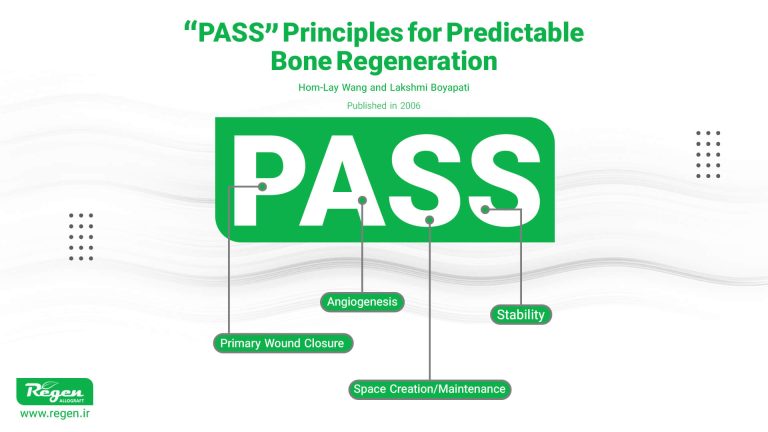
Table of contents
Introduction
The process of Guided Bone Regeneration (GBR) is considered one of the key techniques in periodontology and implantology surgeries. In this process, depending on the morphology of the bone defect, allografts (human bone graft products) and collagen membranes can be the first choice for achieving successful results in bone regeneration treatments.
In this article, we examine the PASS principles, which are used to predict the success of bone regeneration in the GBR technique, as presented in a 2006 article published in the scientific journal Implant Dentistry. By utilizing the principles of Primary wound closure, Angiogenesis, Space creation/maintenance, and wound/graft Stability, the predictability of treatments has significantly increased.
Allografts such as bone powder and granules, as scaffolds used in bone grafting, provide the necessary space for new bone growth. By using mineralized and demineralized allografts, bone-forming cells are effectively stimulated to create new bone in the defect area.
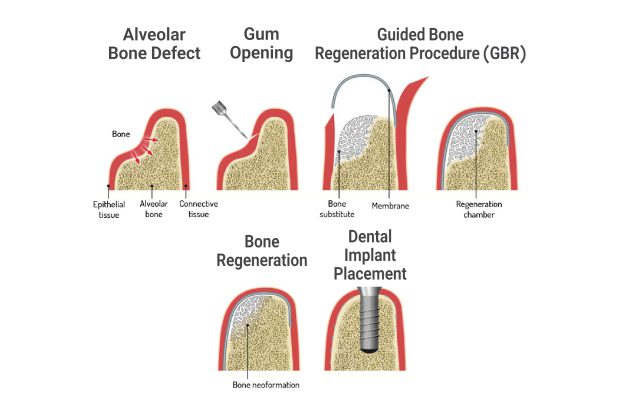
Collagen membranes, such as acellular dermal allografts, pericardium membranes, and fascia membranes, are also effective in conjunction with bone powder to prevent the ingrowth of soft tissues into the bone defect area. In addition to preserving the environment for bone growth, these membranes accelerate the bone regeneration process with physiological properties such as hemostasis and cell adhesion.
Bone allografts and collagen membranes are used, especially in cases where a larger bone volume is needed than the patient’s existing condition allows for implant placement, to properly maintain space for bone formation and prevent membrane collapse. These products significantly increase the success rate of bone regeneration treatments, and patients with large bone defects can achieve more favorable outcomes.

Primary Wound Closure: The Foundation of Success in Bone Regeneration
Primary wound closure in the GBR (Guided Bone Regeneration) technique is one of the crucial principles for creating an undisturbed environment that allows the bone regeneration process to proceed without external influences such as bacteria or mechanical damage. Many scientific studies, including research conducted by Machtei, have shown that when membranes are left exposed to the oral environment, they have a negative impact on treatment outcomes. In cases where the membranes are properly covered, a bone increase of 3.01mm around the implant was observed, which indicates the importance of proper wound closure.
Similar studies by Simion et al. also showed that if the membranes remain covered for 6-8 months without exposure, the rate of bone regeneration reaches 99.6%, while early membrane exposure causes a sharp decrease in this rate to 48.6%
Angiogenesis: A Key Process in Bone Regeneration
Angiogenesis, meaning the formation of new blood vessels, is essential for delivering oxygen and nutrients to the wound site and facilitating the 1 entry of bone-forming cells into the injured area. Various studies, particularly those conducted by Buser and colleagues, have shown that creating cortical perforations in bone significantly increases angiogenesis and facilitates the migration of osteogenic (bone-forming) cells to the wound area. This technique, known as the regional acceleratory phenomenon (RAP), increases the rate of bone regeneration by 2-10 times and accelerates the healing process, although there are some disagreements regarding this effect.
Giannobile and colleagues have also shown in research that growth factors such as PDGF and BMPs can act as important catalysts in angiogenesis and osteogenesis. This research suggests that stimulating angiogenesis using these factors, especially in GBR, can contribute to faster and more predictable bone regeneration.
Titanium-reinforced membranes are of particular importance due to their ability to prevent collapse and maintain optimal space in bone regeneration, especially in cases where the bone defect is extensive and the morphology of the bone defect lacks sufficient retaining walls.
In a study conducted by Jovanovic et al., it was shown that the use of titanium-reinforced membranes resulted in a significant increase in bone volume compared to non-reinforced membranes. This research demonstrated positive results in bone regeneration in areas with large defects, where the need to maintain precise space and prevent membrane collapse is crucial. In this study, bone volume increase in areas where reinforced membranes were used was observed to be 1.82 mm to 1.9 mm, while in the control groups, this amount was only 0.53 mm. Despite non-resorbable membranes, especially titanium-reinforced types, allograft bone powders can be the first choice in spaces created under this type of membrane.
Space Creation and Maintenance: A Crucial Role in Bone Regeneration
Creating and maintaining space to prevent the ingrowth of non-osseous tissues into the wound area and providing a suitable environment for osteoblast cell proliferation is a fundamental principle for successful Guided Bone Regeneration (GBR). Barrier membranes are generally used to prevent the ingrowth of epithelial and connective tissue cells into the treatment area and to provide adequate space for bone cell proliferation.
Wound or Graft Stability: The Most Important Factor in Successful Intra-Graft Angiogenesis
Stability in the GBR (Guided Bone Regeneration) technique is divided into two main parts: blood clot stability and implant stability. In many scientific studies, it has been shown that the stability of the blood clot, especially in the early stages of healing, plays a vital role in the formation of granulation tissue and the initiation of the bone formation process. Growth factors such as PDGF (Platelet-Derived Growth Factor) and TGF-β (Transforming Growth Factor Beta) are found in large quantities in the blood clot and are responsible for attracting osteoblasts and initiating the bone formation process.
Improving GBR Outcomes by Adhering to PASS Principles
The use of allografts and collagen membranes as complementary tools in the GBR (Guided Bone Regeneration) process provides an effective solution for treating bone defects and achieving successful bone regeneration. Our company, a pioneer in allograft production, can help dental professionals achieve successful and predictable results by providing high-quality products.
The GBR technique, when adhering to the PASS principles, can be used as a predictable and successful treatment for bone regeneration and providing suitable conditions for dental implant placement. Various clinical studies and research have shown that strict adherence to these principles can significantly increase treatment success rates. In particular, research indicates that the use of reinforced membranes, maintaining adequate space for bone cell proliferation, and promoting angiogenesis can greatly contribute to GBR success in complex areas with bone defects.
By choosing human allografts and collagen membranes for treating bone defects, you contribute to increasing the speed and quality of treatments and ensure a higher percentage of new bone formation with minimal residual particles from the graft material.
Reference:
Title: “PASS” Principles for Predictable Bone Regeneration
Journal: Published in the journal Implant Dentistry, 2006
Authors: Hom-Lay Wang and Lakshmi Boyapati
How useful was this post?
Click on a star to rate it!
Average rating 0 / 5. Vote count: 0
No votes so far! Be the first to rate this post.
Relevant Posts

Free consultation
Do you need counseling?
The professional and specialized team at Allograft is ready to assist you