Using Allografts in Hand Surgery: Tendon Reconstruction Without Donor Site Harvesting
Table of contents
Tendon grafting is a widely accepted approach for tendon defect reconstruction, particularly in orthopedic and reconstructive surgery. While autografts remain the gold standard, tendon allografts offer a promising alternative, especially in cases where autologous tissue is unavailable or insufficient. However, despite their advantages, tendon allografts have not yet seen widespread adoption in upper limb reconstruction.
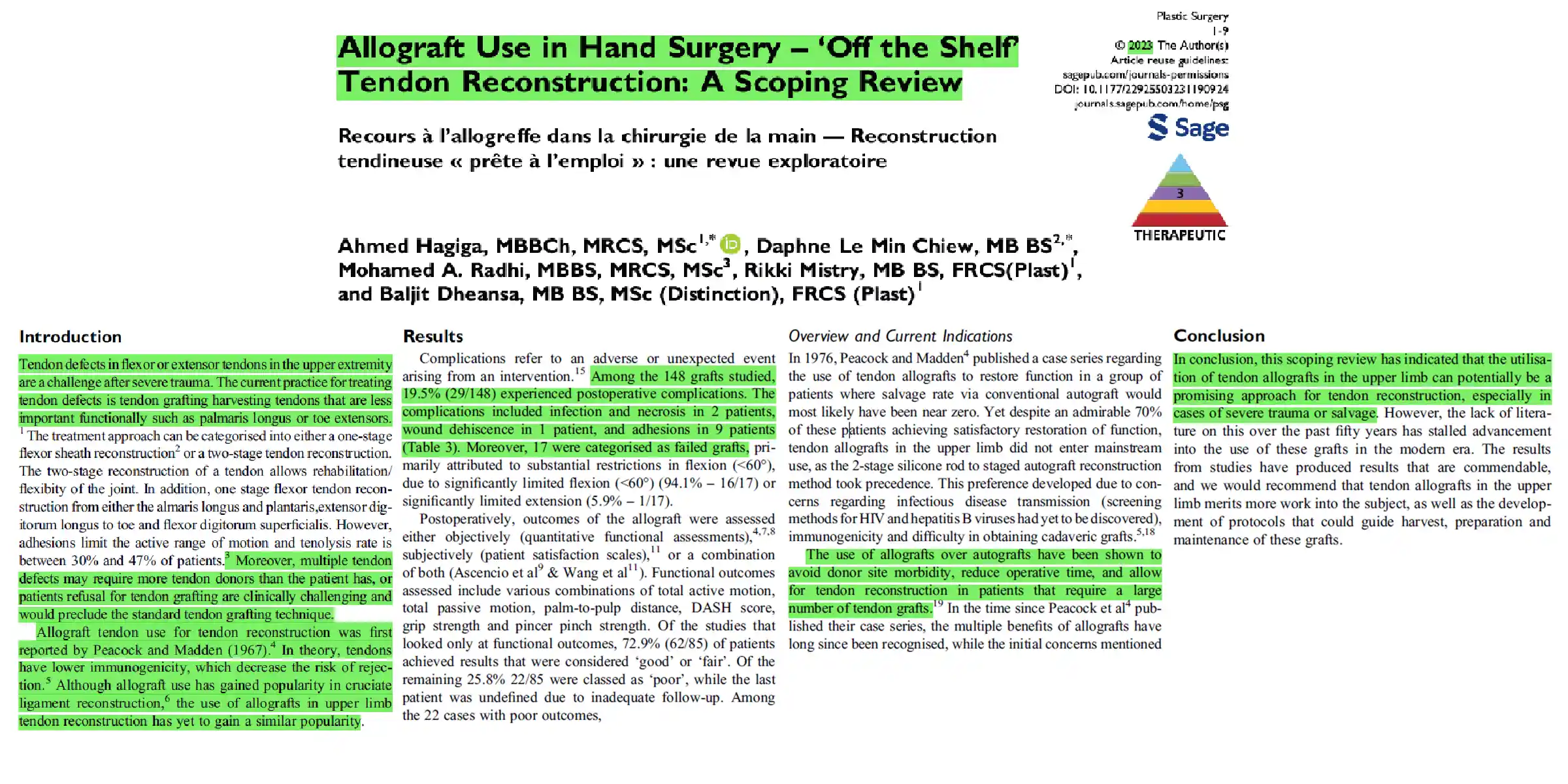
This article summarizes a 2023 scoping review titled “Allograft Use in Hand Surgery – ‘Off the Shelf’ Tendon Reconstruction: A Scoping Review,” which systematically analyzed the current applications of tendon allografts in hand surgery. The review utilized Medline and Scopus to identify relevant studies up to June 2022, focusing on upper limb tendon reconstruction. Eligible studies included randomized controlled trials (RCTs), cohort studies, case-control studies, cross-sectional research, and case reports involving patients who underwent tendon allograft reconstruction.
From the database search, the review identified six eligible studies, covering 116 patients and 148 tendon allografts. Functional outcomes varied, with 72.9% of patients achieving “good” or “fair” results, while 25.8% were classified as “poor.” Patient-reported outcomes indicated that all evaluated individuals were at least somewhat or moderately satisfied with their surgical results.
The findings highlight the potential of tendon allografts as a viable solution for severe tendon injuries in the upper limb. However, further research is essential to assess long-term outcomes, complication rates, rehabilitation protocols, and comparative efficacy against traditional autografts.
Introduction: Challenges and Advances in Upper Limb Tendon Reconstruction
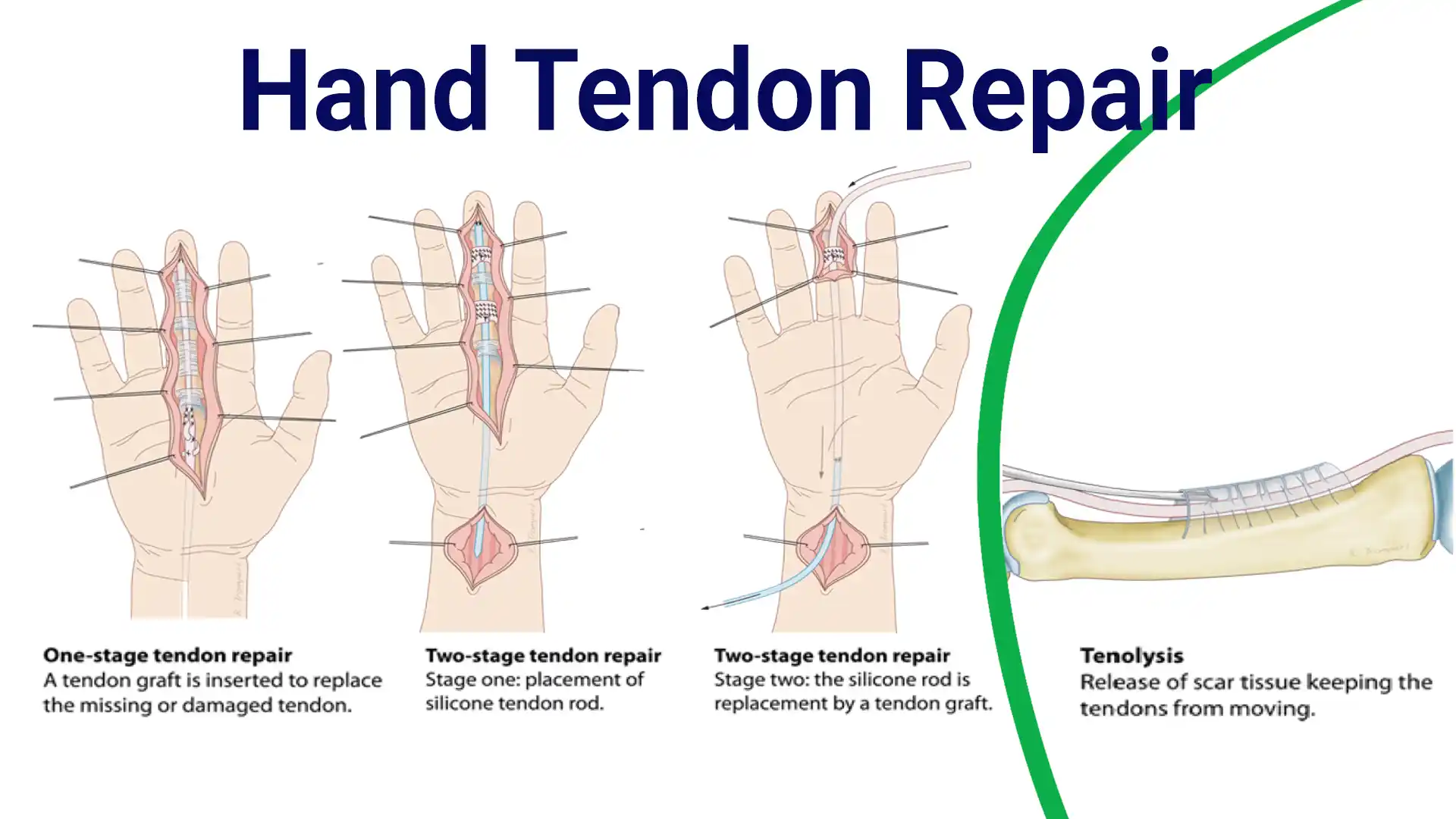
Severe trauma to the flexor and extensor tendons of the upper limb presents a major reconstructive challenge. Traditional treatment methods rely on autograft tendon harvesting, typically using less functionally critical tendons such as the palmaris longus, plantaris, extensor digitorum longus, or flexor digitorum superficialis. Depending on the severity and complexity of the injury, reconstruction strategies are categorized into:
- Single-stage tendon sheath reconstruction, which allows immediate repair but is often limited by adhesion formation, significantly restricting the active range of motion. Tenolysis rates in these cases range from 30% to 47%.
- Two-stage tendon reconstruction, which improves joint flexibility and rehabilitation outcomes but requires a prolonged treatment course.
However, extensive tendon defects may exceed the number of available donor tendons, and some patients may be unwilling to undergo autograft harvesting due to additional surgical risks. This has driven interest in tendon allografts as an alternative solution.
The concept of using tendon allografts for reconstruction was first introduced by Peacock and Madden in 1967. Unlike other allogeneic tissues, tendons exhibit lower immunogenicity, theoretically reducing the risk of graft rejection. While allograft use has gained significant acceptance in anterior cruciate ligament (ACL) reconstruction, its application in upper limb tendon repair remains less widespread.
To evaluate the current role of tendon allografts in upper limb reconstruction, a scoping review was conducted to systematically analyze existing studies. The review aimed to:
- Assess the clinical effectiveness of tendon allografts in hand and wrist surgery.
- Identify gaps in knowledge regarding graft rejection, complications, and functional outcomes.
- Provide insights to guide future research and optimize treatment protocols.
Scoping Review Methodology: Investigating Tendon Allograft Use in Hand Surgery
This scoping review was conducted following the Arksey and O’Malley framework, with strict adherence to the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses for Scoping Reviews) guidelines. To ensure a comprehensive and systematic analysis, two independent reviewers performed structured searches across three major databases—MEDLINE, PubMed, and SCOPUS—from their inception until June 2022. Studies were identified through a multi-step process, including title screening, abstract review, and full-text assessment.
As is standard in scoping review methodology, article quality was not formally assessed, as the primary objective was to map the existing literature rather than conduct a critical appraisal of the evidence.
Study Scope and Key Metrics
The review included 116 patients and 148 tendon allografts, focusing on clinical cases involving:
- Severe tendon trauma
- Congenital tendon deficiencies
- Failed prior tendon reconstruction surgeries
Data extraction focused on functional outcomes, patient satisfaction, postoperative complications, and follow-up periods, providing a broad overview of the current state of tendon allograft applications in upper limb surgery.
Findings from the Scoping Review on Tendon Allografts
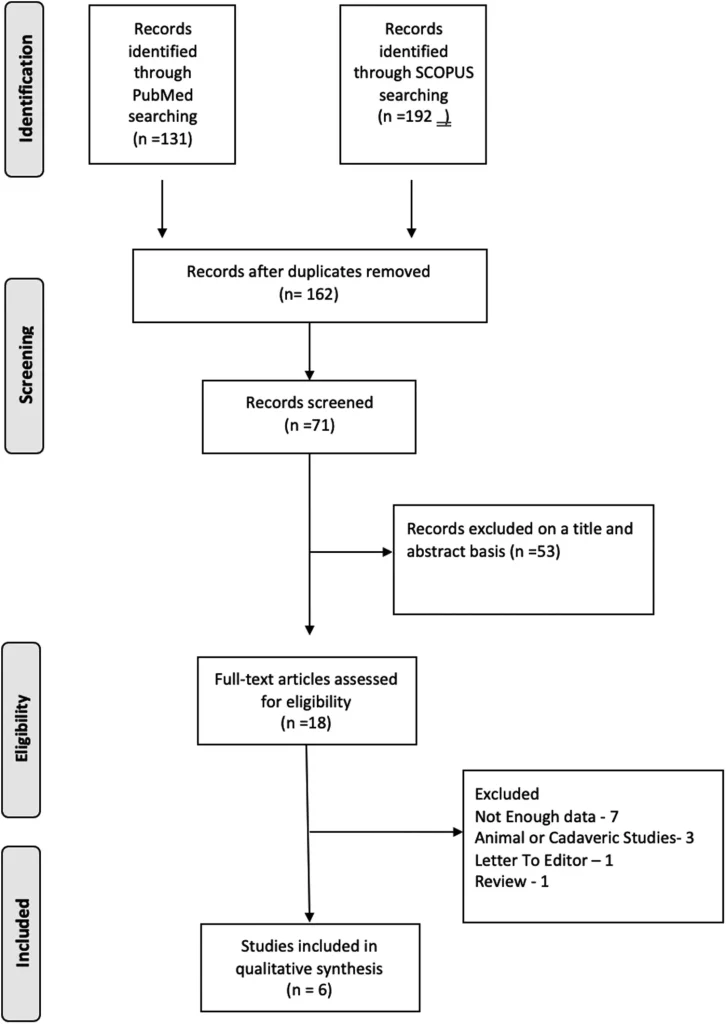
A systematic database search initially identified 323 studies, which were reduced to 162 after duplicate removal. After screening titles and abstracts, 18 articles were deemed potentially eligible, and 6 studies ultimately met the inclusion criteria. Among these:
- 5 studies were case reports or case series.
- 1 study was a retrospective cohort analysis.
- All examined the use of tendon allografts for upper limb tendon reconstruction.
Patient and Injury Characteristics
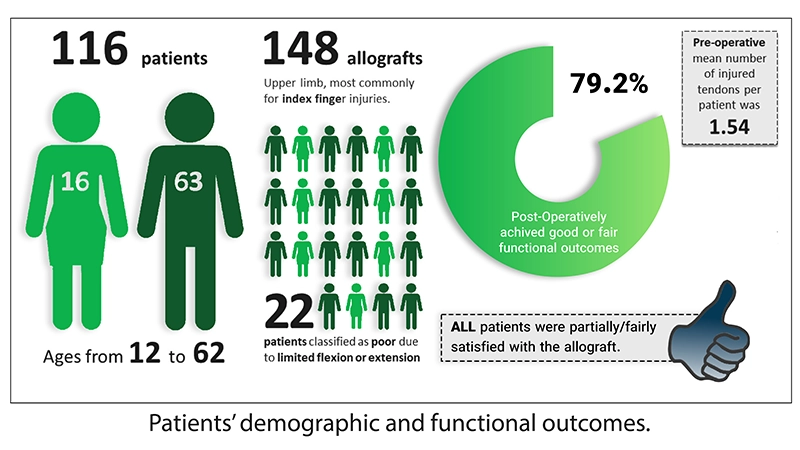
The six studies collectively included 116 patients and 148 tendon allografts, categorized as follows:
- 120 allografts were used for flexor tendon reconstruction.
- 24 allografts were used for extensor tendon reconstruction.
- The index finger was the most frequently reconstructed site (26 patients), while the little finger was the least common (10 patients).
Regarding patient demographics:
- Ages ranged from 12 to 62 years (excluding Iselin, 1976, which lacked demographic data).
- The majority were male (63 patients) compared to female (16 patients).
- The average number of damaged tendons per patient was 1.54, with injuries ranging from 1 to 9 tendons per patient.
- 4 studies focused on patients with failed primary autografts or cases involving severe soft tissue or bone damage.
- Shieh (2012) included patients requiring more tendon material than available from autografts or those preferring allografts over autografts.
- Iselin (1976) did not specify a patient selection criterion.
This review highlights the growing clinical relevance of tendon allografts in reconstructive hand surgery, particularly for complex or multi-tendon injuries where traditional autografts may be insufficient.
Pre-operative assessment plays a critical role in determining the success of orthopedic procedures, particularly in tendon and joint repair using allografts. Various scoring systems—such as the Boyes, Hunter and Salisbury (H&S), and Modified Hand Injury Severity Score (MHISS)—along with functional evaluations like total active motion (TAM), total passive motion (TPM), and fingertip-to-palm distance (FTPD) are commonly utilized to assess hand and tendon injuries before surgery.
Among studies employing these assessment methods, only 6.67% (7/105) of allograft applications were performed on cases classified as “mild” or “good,” indicating that allografts are primarily used in moderate to severe tendon injuries. For instance, in the Ezelin study, the average Boyes grade was 3, signifying joint involvement and reduced mobility. Additionally, 24.3% (9/37) of patients had grade V injuries, representing multisystem trauma involving severe wounds, joint damage, and nerve involvement. In another study, the average Hunter and Salisbury score was V, correlating with extensive soft tissue scarring and joint deterioration, while the MHISS score in Wang’s research averaged 148.9, a stark contrast to the baseline population score of 10.1 (SD ±14.68), indicating severe hand dysfunction.
Post-operative complications, a major concern in orthopedic allograft applications, were observed in 19.5% (29/148) of grafts. These complications ranged from infection, necrosis, and wound dehiscence to adhesions and graft failure. Notably, 94.1% (16/17) of failed grafts were attributed to severe flexion limitations (<60°), while 5.9% (1/17) exhibited significant extension deficits.
To assess surgical success, researchers employed both objective functional measurements (grip strength, pinch strength, DASH score, TAM, TPM) and subjective patient-reported outcomes (pain, stiffness, return-to-work ability, satisfaction). Remarkably, 72.9% (62/85) of patients achieved “good” or “acceptable” functional results, while 100% (58/58) of patients who underwent subjective assessments reported at least partial satisfaction with the allograft procedure.
History and Advancements in Allograft Use for Hand Surgery
The use of tendon allografts in hand surgery dates back to 1967, when Peacock and Madden pioneered their application for complex tendon reconstructions. Their study demonstrated that tendon allografts could restore function in patients with limited recovery prospects, achieving satisfactory outcomes in approximately 70% of cases.
Despite these promising results, two-stage tendon reconstruction with silicone rods soon became the preferred method. This approach involved an initial implantation of a silicone rod, followed by a secondary procedure replacing it with an autograft (a tendon harvested from the patient).
Early barriers to allograft adoption included concerns about disease transmission and immune rejection. However, advancements in sterilization techniques—such as gamma irradiation and strict donor screening protocols—have significantly reduced these risks, making allografts a safer and more viable option in modern reconstructive hand surgery.
Tendon Allograft Harvesting, Preservation, and Storage Protocols
Unlike some orthopedic procedures, a standardized protocol for tendon allograft preparation has not been universally established. Various studies have implemented different techniques for harvesting, preservation, and storage, although most follow a general process that includes:
- Sterile harvesting under controlled conditions
- Cleaning procedures using solutions such as normal saline (± antibiotics), Cialit (a mercury-based antibacterial), or DMSO
- Sterilization, predominantly through gamma irradiation
- Storage, which varies based on medium (sterile plastic bags, antibiotic solutions, or liquid nitrogen) and temperature (room temperature, refrigeration (4°C), freezing (−20°C), or ultra-low freezing (−80°C))
- Pre-surgical processing, ranging from no additional treatment to washing with saline or antibiotic-soaked solutions
- Notably, 21st-century studies increasingly rely on commercial tissue banks, rigorous infection screening, and irradiation-based sterilization to enhance allograft safety and reliability in clinical applications.
Complications and Safety of Tendon Allografts in Hand Surgery
A comprehensive review of six studies on tendon allograft complications in hand surgery revealed low rates of infection and graft-related failures. Across all cases, only two instances of infection or necrosis and one case of wound dehiscence were reported. Notably, no deep infections, immune rejections, or infectious disease transmissions occurred, even in the absence of standardized sterilization, infectious disease screening, or immunosuppressive protocols.
Historically, concerns over infection risks and immune response contributed to the widespread adoption of two-stage tendon reconstruction with silicone rods. However, modern advancements—such as gamma irradiation sterilization and rigorous donor screening—have significantly reduced the risks of pathogen transmission. These improvements have helped establish tendon allografts as a safer and more viable option for complex reconstructive procedures.
Further supporting this, experimental research has demonstrated that tendons are largely acellular, reducing the likelihood of immune rejection. For instance, Wang et al. analyzed immune markers before and after transplantation, reporting no immune response activation in patients with fully functional immune systems who were not receiving immunosuppressive treatment. These findings are consistent with studies in anterior cruciate ligament (ACL) reconstruction, where tendon allografts have been widely used without significant rejection concerns.
Limitations of Current Research
Despite promising outcomes, small sample sizes remain a major limitation in tendon allograft research, particularly in upper extremity surgeries. This review included only 148 tendon allografts, restricting the generalizability of findings. Additionally, limited quality assessment of the studies further reduces the ability to establish standardized clinical recommendations.
Moreover, the majority of reviewed studies consisted of case reports and case series, which inherently lack control over confounding variables, potentially introducing bias into the reported results.
Conclusion and Future Directions
This review highlights the potential of tendon allografts as an effective solution for tendon reconstruction in severe upper extremity injuries. However, limited research over the past five decades has slowed the development of standardized harvesting, processing, and preservation protocols.
Given the encouraging clinical outcomes observed, further research is essential to refine best practices for allograft preparation and establish evidence-based guidelines for their use in reconstructive hand surgery.
What are Tendon Allografts?
Tendon allografts are tendons from a deceased donor that are carefully processed and sterilized to ensure safety and effectiveness. These grafts provide a ready-made solution for tendon reconstruction, eliminating the need for autografts, which require harvesting from the patient’s own body.
Types of Tendon Allografts
- Flexor Tendons: Primarily used for hand and finger reconstruction.
- Extensor Tendons: Less commonly used but are crucial for certain specific injuries in the upper limbs.
- Composite Grafts: Used for complex cases involving multiple tendon and tissue injuries.
Why Choose Tendon Allografts Over Autografts?
Tendon allografts offer significant advantages
- No Donor Site Morbidity: They eliminate the complications associated with harvesting autografts.
- Expanded Availability: They provide options for patients who lack sufficient donor tendons.
- Shorter Operative Times: Particularly in complex cases, they reduce the duration of surgery.
- Viability for Complex Cases: They are ideal for severe injuries, failed autografts, or multiple tendon defects.
hand surgery and tendon reconstruction
Results of Tendon Allograft Research in Hand Surgery: Key Findings
A comprehensive review of tendon allograft outcomes in hand surgery analyzed data from 116 patients and 148 tendon allografts, yielding several important insights:
Functional Outcomes
- 72.9% of patients achieved “good” or “moderate” results, demonstrating substantial restoration of movement and strength.
- Functional metrics included Total Active Motion (TAM), grip strength, and range of motion assessments.
Patient Satisfaction
100% of patients reported at least partial satisfaction, highlighting improvements in hand function, pain reduction, and the ability to return to daily activities.
Complications
The study reported a complication rate of 19.5%, primarily involving adhesions and limited mobility.
Advances in sterilization and surgical techniques have significantly reduced infection risks.
Modern Advances in Tendon Allograft Processing and Preservation
The processing and preservation of tendon allografts have evolved with advanced protocols that ensure higher safety and efficacy:
- Sterilization: Techniques such as gamma irradiation and chemical sterilization are employed to eliminate pathogenic microorganisms.
- Preservation: Cryopreservation at -80°C or deep freezing ensures long-term viability of tendon allografts.
- Screening: Rigorous donor testing ensures that allografts are free from infectious diseases, further enhancing patient safety.
These modern advancements have made tendon allografts a reliable and safer option for tendon reconstruction.
Key Takeaways for Orthopedic Surgeons
Tendon allografts offer a viable alternative for complex tendon reconstructions, especially when autografts are not feasible due to factors like donor site morbidity or tissue scarcity.
Improvements in sterilization, preservation, and screening have significantly enhanced the safety and efficacy of tendon allografts.
Despite promising results, further research and the development of standardized protocols are essential for the widespread adoption of tendon allografts in clinical practice.
References
Allograft Use in Hand Surgery – ‘Off the Shelf’ Tendon Reconstruction: A Scoping Review, 2023, Ahmed Hagiga, Daphne Le Min Chiew, Mohamed A. Radhi, Rikki Mistry, Baljit Dheansa, https://doi.org/10.1177/22925503231190924
How useful was this post?
Click on a star to rate it!
Average rating 5 / 5. Vote count: 1
No votes so far! Be the first to rate this post.
Relevant Posts

Free consultation
Do you need counseling?
The professional and specialized team at Allograft is ready to assist you