Dentistry and Maxillofacial
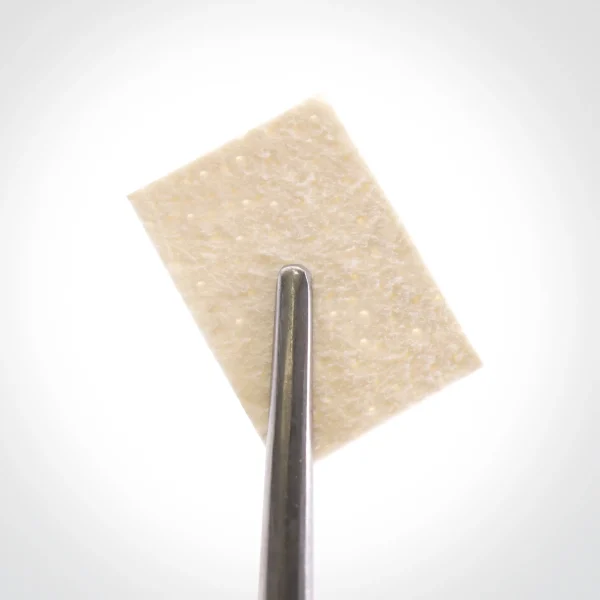
The acellular dermis membrane collagen membrane, contains basement membrane on one of its surfaces. It can provide a dense and impenetrable layer against microorganism and pathogen penetration into deeper layers.
So the membrane surface can stay exposed in high-perfused tissue of the oral cavity. The product origin is the collagen membrane (skin dermal layer), which consists of strong collagen type I and III fibers that strengthen the product, and also elastic fibers causing flexibility. This collagen membrane results in product’s unique features.
Demineralized bone matrix (DBM) putty is a highly specialized bone graft material that has emerged as a valuable tool in the surgical management of bone defects. Derived from human or animal bone that has been processed to remove its mineral components, DBM putty presents a soft, malleable scaffold richly endowed with osteoconductive and osteoinductive properties. These properties enable DBM putty to serve as a platform for bone cell attachment, proliferation, and differentiation, fostering the regeneration of new bone tissue.
DBM putty offers a range of advantages over traditional autografts (bone grafts harvested from the patient’s own body) and allografts (bone grafts sourced from cadavers). Its osteoconductive nature allows it to seamlessly integrate with the surrounding bone, while its osteoinductive capacity stimulates the production of bone-forming proteins, accelerating the healing process.
The biocompatible carrier in which DBM putty is incorporated plays a crucial role in its moldable and easy-to-form nature. This carrier, typically a combination of collagen and alginate, provides the putty with its desired consistency, allowing surgeons to precisely shape and contour it to fill bone voids of various sizes and configurations. The carrier also contributes to the overall bioactivity of DBM putty, enhancing its ability to promote bone regeneration.
The product is processed from human Fascia Lata and is available as lyophilized, radiated products in various sizes. Due to its flexibility, adhesiveness, and biocompatibility, it can easily be used at the operation site and causes volume enhancement and mechanical strength.
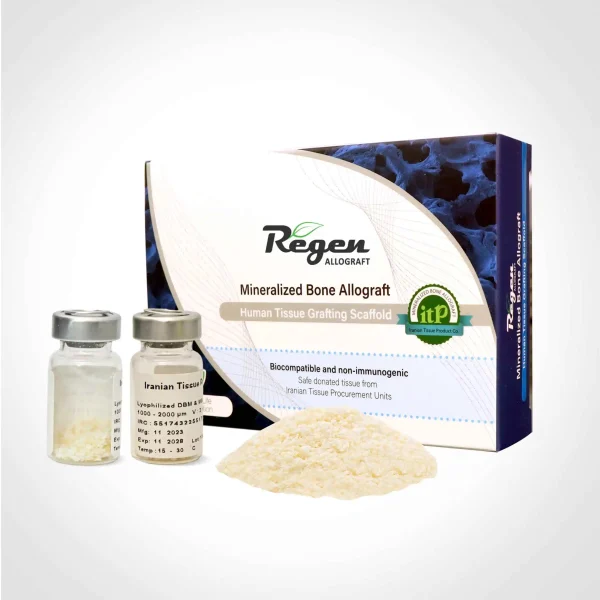
Particulated bone allografts, derived from human bone tissue, are biomaterials used to fill bone defects and promote bone regeneration. They come in various particle sizes, each offering unique properties and applications.
Powdered allografts, the smallest particles, possess high integration capabilities and are suitable for small defects. Granule and crushed allografts are larger in size, serving as a foundation for bone regeneration and can be used as fillers or for augmentation.
Chip allografts, the largest among particulated bone grafts, provide a bone scaffold, making them ideal for larger defects or augmentation.
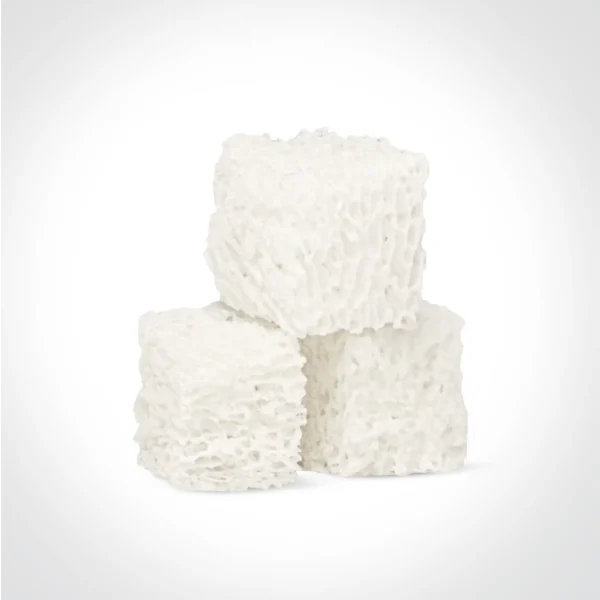
Freeze-dried bone allograft as Bone grafting such as Cube, Matchstick and Block forms has revolutionized orthopedic and maxillofacial surgeries, offering distinct advantages due to their unique compositions. Cube and Matchstick configurations consist solely of cancellous bone, while block formations comprise a core of cancellous bone enveloped by a cortical surface. These allograft are meticulously processed to decellularization and ensure sterilization. The resulting grafts provide essential structural support and seamlessly integrate with the recipient’s bone, promoting the formation of new bone.
Cube and block bone allografts effectively address osseous deficiencies caused by various conditions, from post-traumatic injuries to degenerative diseases and reconstructive procedures. In dental implantology, they serve as a reliable scaffold for augmenting deficient mandible and maxilla structures and facilitating successful implant placement. Moreover, in reconstruction surgeries, these grafts significantly contribute to restoring maxillofacial and skeletal, enabling patients to regain both physical form and function.
Ongoing refinement of bone grafting techniques, along with continued research and innovation, will further enhance the applications and outcomes of cube and block bone allografts, elevating the standard of care in orthopedic and maxillofacial surgeries.
The acellular dermis membrane collagen membrane, contains basement membrane on one of its surfaces. It can provide a dense and impenetrable layer against microorganism and pathogen penetration into deeper layers.
So the membrane surface can stay exposed in high-perfused tissue of the oral cavity. The product origin is the collagen membrane (skin dermal layer), which consists of strong collagen type I and III fibers that strengthen the product, and also elastic fibers causing flexibility. This collagen membrane results in product’s unique features.